What You Need to Know
Designed especially for UC employees and retirees not enrolled in Medicare, UC Care (administered by Anthem Blue Cross) offers two tiers of in-network coverage: UC Select and Anthem Preferred.
Have questions or need help?
How it works
See the plan comparison chart [PDF] for more coverage details.
Three tiers of coverage: Your cost for care is based on where you receive services.
- Tier 1: UC Select. Available only in California. Features no deductible and set copays for most covered services when you get care from UC physicians and health centers and some other select providers. Every campus — even those without a UC health center — has access to UC Select providers. Tier 1 is focused on primary care and hospital services, and some specialty care. Not all services and provider types are available at the Tier 1 benefit. Provider and service types not available through Tier 1 are likely covered through the Tier 2 (Anthem Preferred) benefit.
- Tier 2: Anthem Preferred. Offers a wider range of providers and facilities, with access to more than 62,000 providers statewide. You must meet an annual deductible, and then the plan pays most of the cost of services received.
- Tier 3: Out-of-network. You can also choose to receive care from out-of-network providers. However, your costs will be significantly higher, and you’ll have to file claims. See the plan comparison chart [PDF] for more details about your cost for out-of-network care.
You can also choose to receive care from out-of-network providers. However, your costs will be significantly higher, and you’ll have to file claims. See the plan comparison chart [PDF] for more details about your cost for out-of-network care.
Did you switch from the UC Health Savings Plan to another medical plan?
No-cost preventive care
Preventive care, including services such as screenings, immunizations and exams for you and all covered family members when you see an in-network provider. (Out-of-network preventive care covered at 50% after the out-of-network deductible.) Learn more about covered preventive care services.
What you pay for care
Deductible
- UC Select providers: $0
- Anthem Preferred providers: $500 (for individual coverage) or $1,000 (for family coverage)
- Out-of-network provider: $750 (for individual coverage) or $1,750 (for family coverage)
Cost of care:1
- UC Select providers: $30 copay for most office visits and other outpatient services.
- Anthem Preferred providers: After your deductible of $500, you pay 30% of the cost of most covered services; there is no deductible for preventive care
- Out-of-network provider: After your deductible, you pay 50% of the cost of most covered services
Out-of-pocket maximum
This limits the amount you’ll pay for covered services during the year. After you meet the out-of-pocket maximum,1 Anthem pays 100% for most covered medical services and Navitus pays for 100% of most prescription drugs, for the rest of the year.
- UC Select providers: $6,100 (for individual coverage) or $9,700 (for family coverage)
- Anthem Preferred providers: $7,600 (for individual coverage) or $14,200 (for family coverage)
- Out-of-network providers: $9,600 (for individual coverage) or $20,200 (for family coverage)
See the plan comparison chart [PDF] for more coverage details.
1. Out-of-pocket costs for UC Select / Anthem Preferred (in-network) services cross-accumulate (i.e., they count toward each other). Out-of-pocket costs for out-of-network services do not count toward the UC Select / Anthem Preferred (in-network) out-of-pocket max or the Anthem Preferred deductible.
No surprises
Did you know that if you receive emergency care or are treated by an out-of-network doctor or specialist at a hospital or ambulatory surgical center in your plan’s network, you are protected from surprise billing?
Behavioral health
You and your covered family members can use behavioral health benefits for sessions with counselors, psychologists or psychiatrists for mental health services and substance use treatment. If you need help finding a provider and booking and appointment, call Accolade at (866) 406-1182 Monday–Friday, 5 a.m.–8 p.m. PT. You can also speak to a therapist or psychologist virtually through Accolade Care Telehealth and Virtual Visits.
Prescription drugs
Your prescription drug coverage includes medications that are part of the Navitus formulary. You can view the formulary, preview drug costs and search for pharmacies on the Navitus portal. For personalized information about coverage and claims, log into the Navitus member portal.
DOWNLOAD THE NAVITUS APP
The Navitus app offers mobile access to your digital ID card to view drug prices, find local pharmacies, and more.
At preferred pharmacies: Fill up to a 90-day supply through select UC Medical Center pharmacies, Costco, CVS, Safeway/Vons, Walgreens, Walmart, and Costco mail order. Log in to the Accolade digital member portal to view the complete list of network pharmacies and find a pharmacy near you.
- Tier 1 (preferred generics and some lower-cost brand: $10 (30-day supply) or $20 (31–90-day supply)
- Tier 2 (preferred brand products and some high-cost non-preferred generics): $30 (30-day supply) or $60 (31–90-day supply)
- Tier 3 (non-preferred products, including some high-cost non-preferred generics): $50 (30-day supply) or $100 (31–90-day supply)
- Tier 4 (specialty): 30%, up to $150 maximum (30-day supply)
- Drugs covered by the Affordable Care Act: $0, including contraceptive drugs and devices, over-the-counter smoking cessation products and prescription drugs, and diabetes supplies (excluding syringes, needles and non-formulary test strips).
At all other Navitus in-network pharmacies (participating pharmacies), you pay:
- Tier 1 (preferred generics): $10 (30-day supply); $20 (31–60-day supply); $30 (61–90-day supply)
- Tier 2 (preferred brand): $30 (30-day supply); $60 (31–60-day supply); $85 (61–90-day supply)
- Tier 3 (non-preferred): $50 (30-day supply); $100 (31–60-day supply); $130 (61–90-day supply)
At out-of-network pharmacies, you pay 50% of the allowable cost.
Mail order: Fill up to a 90-day supply of maintenance medications (those taken on an ongoing basis to treat chronic conditions like asthma, diabetes, high blood pressure and high cholesterol) through the Costco Mail Order Pharmacy. (You do not need to be a Costco member.) Start a new prescription and request refills online or use the mail order form [PDF], and your prescription will be delivered to you by mail. Learn more about how to set up your online account and order through mail order [PDF].
Specialty medications: You can fill prescription drugs used to treat complex conditions through either Lumicera Health Services or select UC pharmacies [PDF]. To get started with Lumicera, visit the website or call them at (855) 847-3553, or work with your provider to use a UC pharmacy. Lumicera offers free delivery to your home or other locations.
Money-saving options:
- Tablet splitting: Buy fewer tablets by breaking a higher-strength drug tablet in half to deliver the same prescribed dose as a full tablet. For medications that can easily be cut in half without compromising efficacy, you can save up to 50% on out-of-pocket costs by having your doctor write a prescription for double the strength (e.g., 20 mg instead of 10 mg) and simply splitting the tablets in half.
Coverage restrictions:
- Brand-name drug penalty: When a generic drug is available and you or your physician chooses the brand-name drug, you must pay the tier 3 (non-preferred) copay plus the difference between the cost of the brand-name drug and the generic equivalent. If a prior authorization is approved for a medical necessity exception, you will pay the Tier 3 (non-preferred) cost.
- Prior authorization: Generally, your doctor must show that a particular drug is medically necessary. You or your physician will need to get approval from Navitus before the prescription can be filled. Log in to the Accolade digital member portal to learn more about prior authorization.
- Quantity limits: Taking too much medication or using it too often isn’t safe and may even increase your costs. If you refill a prescription too soon or your doctor prescribes an amount higher than recommended guidelines, the Navitus pharmacy system will reject your claim. If your doctor believes your situation requires an exception, the doctor can contact Navitus to request prior authorization review.
- Step therapy: In some cases, if your doctor prescribes a more expensive drug to treat your medical condition when a lower-cost alternative is available, Navitus requires you to first try the lower-cost drug before it will cover another drug for that condition. This includes medications used to treat ADHD, diabetes, high cholesterol and multiple sclerosis.
What is a formulary?
What is a formulary?
A formulary is an extensive list of safe, effective medications covered by a health plan. Every pharmacy benefit manager (Navitus, for the UC PPO plans) uses its own formulary and it changes over time as new drugs enter the market and brand-name patents expire. Generally, if drugs aren’t on the formulary, they aren’t covered by the plan.
The Navitus formulary is divided into four tiers. The lowest-cost drugs (mostly generic) are in Tier 1. The highest-cost drugs (specialty) are in Tier 4.
What does this look like?
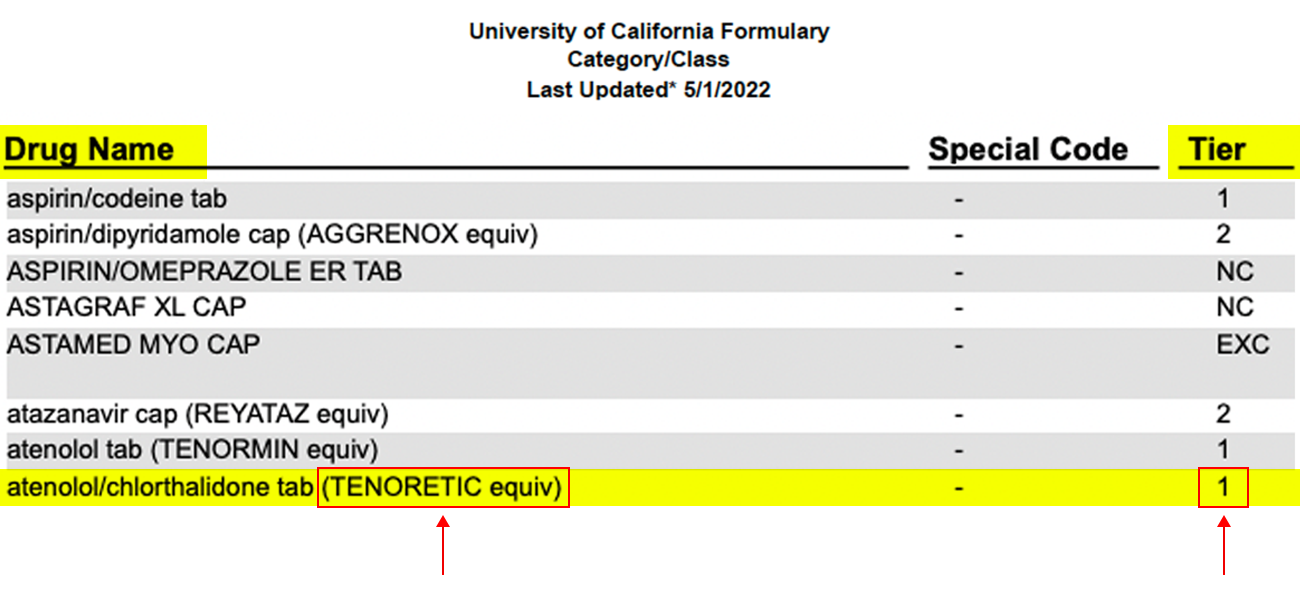
Say you are newly diagnosed with high blood pressure and your doctor prescribes atenolol/chlorthalidone to treat it. A quick scan of the formulary shows atenolol/chlorthalidone is a generic equivalent for the brand-name drug Tenoretic. It also classifies atenolol/chlorthalidone as a Tier 1 medication, so you know what you’ll pay.
The formulary also will show if any restrictions and rules apply, such as prior authorization, quantity limits or step therapy.
Before filling a prescription, first find out if the drug is covered. A quick search of the Navitus formulary will tell you. Download the Navitus app to have the formulary with you at the doctor’s office. If the drug the doctor recommends isn’t listed, you can look for alternatives in real time. If you don’t see the drug on the formulary, you or your doctor can contact Navitus Customer Care at (833) 837-4308 for help.
If there’s a generic version of a drug you are prescribed and your doctor or you choose the brand-name drug instead, you’ll pay a penalty.
2025 formulary updates
2025 formulary updates
April 2025
| Drug name | Change type |
|---|---|
| EVRYSDI TAB | Add to specialty tier |
| XROMI SOLN | Add to Tier 3 |
| galantamine ER cap | Move to Tier 1 |
| OXYTROL PATCH (OTC) | Move to Not Covered |
| renaphro cap | Move to Not Covered |
| dialyvite tab | Move to Not Covered |
| selenium sulfide lotion | OTC no longer covered |
| folbee tab | Move to Not Covered |
| niacin tab | OTC no longer covered |
| niacinamide tab | OTC no longer covered |
| phenazopyridine tab 95mg | OTC no longer covered |
| AZO URINARY TAB | OTC no longer covered |
| phenazopyridine tab 99.5mg | OTC no longer covered |
| phenazopyridine tab 97.5mg | OTC no longer covered |
| NIZORAL A-D SHAMPOO | OTC no longer covered |
| SLO-NIACIN TAB | OTC no longer covered |
| NIACIN TR TAB | OTC no longer covered |
| niacin CR tab | OTC no longer covered |
| NIACIN TR CAP | OTC no longer covered |
| niacin cap | OTC no longer covered |
| diphenhydramine cap 50mg | Move to Not Covered |
| diphenhydramine cap 50mg | Move to Not Covered |
| ALCOHOL SWABS | OTC no longer covered |
| SPS | Move to Not Covered |
| METHYLDOPA TAB | Move to Tier 3 |
| APAP/CODEINE SOLN | Move to Tier 2 |
| AMOXICILLIN/CLAVULANATE CHEW TAB | Move to Tier 2 |
| CEFADROXIL TAB | Move to Tier 2 |
| NEFAZODONE TAB | Move to Not Covered |
| NEOMYCIN/POLYMYXIN/HYDROCORTISONE OPHTH SOLN | Move to Tier 2 |
| ISOSORBIDE MONONITRATE TAB | Move to Tier 3 |
| nebivolol hcl tab | Move to Tier 1 |
| rasagiline tab | Move to Tier 2 |
| colchicine tab | Move to Tier 1 |
| zolpidem ER tab | Move to Tier 1 |
| omega-3-acid ethyl esters cap | Move to Tier 1 |
| potassium citrate CR tab | Move to Tier 1 |
| ranolazine tab | Move to Tier 1 |
March 2025
| Drug Name | Change type |
|---|---|
| ADALIMUMAB-ADAZ INJ | Move to Not Covered |
| FANAPT TAB | Move to Not Covered |
| FANAPT TITRATION PACK | Move to Not Covered |
| VERAPAMIL CR CAP, VERELAN CAP | Move to Not Covered |
| VERAPAMIL SR CAP 360MG | Move to Not Covered |
| GELNIQUE | Remove from formulary- No longer on the market |
February 2025
| Drug Name | Change type |
|---|---|
| NEFFY SPRAY | Add to Tier 2 |
| BESREMI INJ | Add to specialty tier |
| APRETUDE SUSP | Add to $0 tier |
| METHITEST TAB | Move to Not Covered |
| sunitinib malate cap | Add quantity limit |
| ERIVEDGE CAP | Add quantity limit |
| ODOMZO CAP | Add quantity limit |
| TEMPO SMART BUTTON | Add to Tier 2 |
| HUMALOG TEMPO PEN | Add to Tier 2 |
| LYUMJEV TEMPO PEN | Add to Tier 2 |
| INLYTA TAB 1MG | Add to specialty tier |
| FIRST OMEPRAZOLE SUSP | Move to Not Covered |
| esomeprazole DR granule pack | Add to tier 3 |
| LANSOPRAZOLE SUSP | Move to Not Covered |
| lansoprazole odt | Add to tier 3 |
| eluryng vaginal ring | Add to $0 tier |
| NUVARING | Move to Not Covered |
| XPHOZAH TAB | Add to specialty tier |
| SOLU-CORTEF INJ 100MG | Add to tier 2 |
| ABSTRAL SL TAB | Move to Not Covered |
| ACTIQ LOZENGE | Move to Not Covered |
| FENTANYL CITRATE LOLLIPOP | Move to Not Covered |
| fentanyl citrate lollipop | Move to Not Covered |
| FENTORA TAB | Move to Not Covered |
| FENTANYL BUCCAL TAB | Move to Not Covered |
| LAZANDA NASAL SPRAY | Move to Not Covered |
January 2025
| Drug Name | Change type |
|---|---|
| OJEMDA TAB | Add to Specialty Tier |
| OJEMDA SUSP | Add to Specialty Tier |
| XOLREMDI CAP | Add to Specialty Tier |
| REZDIFFRA TAB | Add to Specialty Tier |
| WINREVAIR INJ | Add to Specialty Tier |
| VOYDEYA TAB | Add to Specialty Tier |
2024 formulary updates
2024 formulary updates
December 2024
| Drug Name | Change Type |
|---|---|
| TAZORAC CREAM | Add to Tier 3 |
| FEMLYV TAB | Add to $0 tier |
| TREMFYA INJ 200MG/2ML | Add to specialty tier |
| COMBIPATCH | Add to Tier 2 |
| tiopronin tab delayed release | Add to Tier 1 |
| ONDANSETRON TAB | Move to Not Covered |
| disulfiram tab 500mg | Move to Not Covered |
| OXYCODONE TAB | Move to Not Covered |
| JYNNEOS INJ | Add to $0 Tier |
| OXBRYTA TAB | Move to Not Covered |
November 2024
| Drug Name | Change Type |
|---|---|
| ELMIRON CAP | Move to Not Covered |
| FUZEON INJ | Move to Not Covered |
October 2024
| Drug Name | Change Type |
|---|---|
| LIVMARLI SOLN 19MG/ML | Add to specialty tier |
| TALTZ INJ 20MG/0.25ML TALTZ INJ 40 MG/0.5ML | Add to specialty tier |
| LIRAGLUTIDE SOLN PEN-INJECTOR | Add to Tier 2 |
| VICTOZA INJ | Add to Tier 2 |
Women’s health
All UC PPO plans offer a range of comprehensive clinical resources for every stage of a woman’s life, including no-cost preventive care, family planning and midlife health. Learn more about women’s health services.
Coverage for COVID testing
Provider-ordered tests: PCR testing is covered based on your plan’s benefits. You pay 20% of the cost after the $1,650 (individual)/$3,300 (family) in-network deductible.
Over-the-counter (OTC) tests: Effective Jan. 1, 2025, OTC tests are no longer covered. For any tests purchased in 2024, you have one year from the date of purchase to upload a claim form and receipts to Accolade's secure messaging system for reimbursement.
- Complete sections 1 and 2 of claim form and sign where indicated.
- Log in to your Accolade account through the Accolade app or Accolade digital member portal.
- Select "Messages" followed by "Bill & Claims" to begin your secure submission.
- A new message will appear. Select the paperclip to upload your claim form and receipt. Please clearly state that this is a claim for OTC COVID from 2024 then select "Send".
Claim processing can take up to 45 days. If you do not receive your reimbursement after 45 days or have any questions about your submission, contact Accolade at (866) 406-1182 for help.
Find care
The UC PPO plans give you a range of options to get care when you need it—from in person to virtual care (telehealth), and urgent care and emergency services through University of California Health Providers, the Anthem provider network, and Accolade Virtual Care and 2nd.MD. (Your primary care doctor and specialists may also offer virtual appointment options. Contact their office for more information.) You’re even covered when you’re traveling out of state or out of the country. Find the right care for your need.
Referrals and prior authorizations
Some specialists — and specialty treatment centers (like nephrology or infusion) — may require a referral from your primary care doctor or prior authorization from Accolade before you can make an appointment. When scheduling an appointment, call Accolade at (866) 406-1182, Monday–Friday, 5 a.m.–8 p.m. PT to ask if a preservice review or precertification is required prior to your initial visit.
Certain services, such as a planned surgery with an overnight hospital stay, require prior authorization from Accolade. If you have a procedure scheduled or a condition that will require treatment, you may need a preservice review. For assistance, call Accolade at (866) 406-1182, Monday–Friday, 5 a.m.–8 p.m. PT.
Filing claims
Medical and behavioral health
When you see in-network providers, there are no claim forms to fill out. Your provider handles all the paperwork.
If you see an out-of-network provider for medical or behavioral health services or use an out-of-network pharmacy, it's up to you to submit a claim for reimbursement for services received or prescriptions.
The easiest way to file an out-of-network claim is to start with Accolade. Call (866) 406-1182 (Monday–Friday, 5 a.m.–8 p.m. PT) or visit the digital member portal. Accolade will direct you to the correct forms and answer any questions you have.
If you prefer, you can file out-of-network medical and behavioral health claims directly with Anthem through the Anthem member portal or the Sydney Health app. Download it through the App Store or Google Play.
Pharmacy
When you fill prescriptions at Navitus network pharmacies, there are no claim forms to fill out. Your pharmacy handles all the paperwork. If you use an out-of-network pharmacy, it's up to you to submit a claim for reimbursement for services received or prescriptions. The easiest way to file an out-of-network claim is through the Navitus member portal.
Get help
For questions about medical coverage, claims, finding providers and more, start with Accolade. Call (866) 406-1182 (Monday–Friday, 5 a.m.–8 p.m. PT) or visit the Accolade website.
For questions about prescription drug coverage and costs, call Navitus Customer Care at (833) 837-4308 or visit the Navitus member portal.
Anthem Blue Cross Life and Health Insurance Company is the claims administrator for UC PPO Plans. On behalf of Anthem Blue Cross Life and Health Insurance Company, Anthem Blue Cross processes and reviews the medical, pharmacy and behavioral health claims submitted under the PPO plans. Anthem Blue Cross Life and Health Insurance Company is an independent licensee of the Blue Cross Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. Navitus is an independent company providing pharmacy benefit management services on behalf of the University of California for the PPO plans. Accolade is an independent company providing benefits advocacy services on behalf of the University of California for the PPO plans. Health Net is the claims administrator for the UC Blue & Gold HMO. Health Net processes and reviews the medical, pharmacy and behavioral health claims submitted under the UC Blue & Gold HMO. All plan benefits are provided by the Regents of the University of California. The content on this website provides highlights of your benefits under the UC non-Medicare PPO Plans plans and the Blue & Gold HMO. The official plan documents and administrative practices will govern in any and all cases.
